Risk Communication in Medical Imaging
By Prof Dr. Graciano Paulo, Professor of Medical Imaging & Radiotherapy, IPC-ESTeSC, Coimbra Health School, Head of the WHO Collaborative Centre for Radiation Protection and Health IPC ESTeSC, Coimbra Health School, Past President, European Federation of Radiographer Societies, Coimbra, Portugal
An increasing volume of medical imaging procedures combined with a demand for more rapid access to diagnostic services, is putting high pressure on medical imaging departments. Because of that a communication strategy should be adopted, to explain the procedure in an understandable manner, adapted to patient social and economic characteristics, giving the adequate information for him/her to be able to make a proper decision.
We need to incorporate into our daily practice the understanding of the concept that the 21st century patients have higher expectations and are becoming more demanding, as they are progressively being part of the process and therefore have access to information, allowing them to make better informed choices.
It’s important to be aware that a patient’s listening is motivated by universal needs: The need for compassion; the need to be heard; the need to be recognised. From a tone of voice or acknowledgment, the patient can readily hear if the white coat standing in front of him/her is someone who can care enough to listen.
Medical imaging departments present an excellent test environment to study interventions to enhance patient satisfaction as: a) the imaging environment is highly complex, and workflow and time schedule constraints are extensive; b) there is a wide spectrum of patients referred from multiple clinical specialties whose conditions vary in acuity, ranging from outpatients undergoing routine examinations to critically ill patients undergoing emergency imaging studies.
Research indicates that training Radiologists and Radiographers to make simple modifications in their language and behaviour during patient care, can significantly impact patient satisfaction, which can impact quality-of-care. Authors have also described that radiographers have reported that as the use of technology has increased, traditional radiographer communication has decreased, mainly due to the fact that the implementation of picture archiving and communication systems (PACS), electronic health records (EHR) and digital imaging shorten turnaround times and increase medical imaging department volume without a subsequent staffing increase.
Radiographers usually are the only ones that are in contact with patients and might notice duplicate or inappropriate examinations before they occur and the ones to be asked about the risk. Therefore, its crucial to develop guidelines with clearly defined roles and responsibilities on how to communicate risks in a harmonised way, to avoid patient misinterpretation in their imaging clinical pathway.
Teamwork is needed wherever multiple individuals with multiple skills are required to work interdependently to achieve a favourable outcome. This means that teamwork is absolutely critical in the management of patients, since healthcare is a complex activity, which needs many different types of professionals, with different knowledge, skills and competences and with specific roles.
One individual working alone cannot achieve the target of taking care of a patient and from the concept defined in 1926 by Francis Peabody that “the secret of the care of a patient is caring for the patient” we moved nowadays to: “the real secret of the care of a patient is teamwork”.
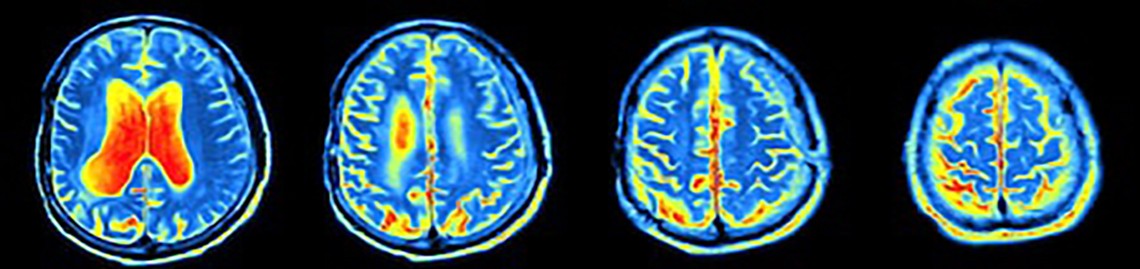
According to the WHO, communicating radiation risk in paediatric imaging, the major challenge in communicating the benefits and risks of medical imaging procedures that use ionizing radiation is the existence of insufficient awareness and understanding of radiation protection issues by health professionals. Research has shown that there is widespread underestimation of doses and risks. There is a need to ensure that all referring medical practitioners have sufficient background, education and resources to communicate clearly and effectively about the benefits and risks of imaging procedures.
Effective communication with patients and caregivers is increasingly recognised as critical to patient-centred care, and an important component of effective healthcare delivery. This is also true in the paediatric population related to communicating radiation benefits and risks from medical imaging. However, the quantity and quality of communications training that most healthcare professionals receive, and the lack of resources available to them, present a hurdle to effective communication in these settings.
Communication with patients and caregivers is one of the requirements of the new International Basic Safety Standards for Protection against Ionizing Radiation and for the Safety of Radiation Sources. Communication of benefits and risk of medical interventions forms the basis of good medical practice. There are several stakeholders who have an interest in providing high-quality care to the patient undergoing imaging procedures. It is essential for them to participate in the risk–benefit dialogue.
In conclusion, despite the pressure on medical imaging departments to produce more, we must dedicate time in communicating effectively with our patients.
Because each patient has his/her own needs and perceptions, we need to be able to identify those needs and perceptions and adapt our messages accordingly, keeping them simple, objective and understandable.
We need to engage with our patients, comfort them, talk with them and show that we particularly care about them.